Although extremely abnormal, a rare few who got Covid shots make antibodies that spark clots
The following written content from Erin Garcia de Jesús
Evidence is building that an uncommon immune response is behind dangerous, but incredibly rare, blood clots associated with some COVID-19 vaccines. But the good news is that there is a test doctors can use to identify it and get patients the right care.
A small number of people out of the millions vaccinated with AstraZeneca’s or Johnson & Johnson’s COVID-19 shots have developed severe blood clots, such as ones in the sinuses that drain blood from the brain (SN: 4/7/21; 4/13/21). A few have died.
Studies suggest that some inoculated people develop an immune response that attacks a protein called platelet factor 4 or PF4, which makes platelets form clots. Those platelets get used up before the body can make more. So these patients wind up with both the rare clots and low levels of blood platelets.
Of 23 patients who received AstraZeneca’s jab and had symptoms of clots or low platelets, 21 tested positive for antibodies to PF4, researchers report April 16 in the New England Journal of Medicine. Of those, 20 people developed blood clots. The finding adds to previous studies that found the same antibodies in additional patients who got AstraZeneca’s shot and had the dangerous clots.
Five out of six women who had clots after receiving Johnson & Johnson’s shot in the United States also had PF4 antibodies, health officials said April 14 during an Advisory Committee on Immunization Practices meeting. That advisory group to the U.S. Centers for Disease Control and Prevention is assessing what needs to be done to lift a temporary pause on administering the Johnson & Johnson jab that was prompted by blood clot concerns (SN: 4/13/21). One man had developed brain sinus clots during the shot’s clinical trial and a seventh case is under investigation, the pharmaceutical company said during the meeting.
“Because we are aware of this syndrome… we know how to treat it,” says Jean Connors, a clinical hematologist at Harvard Medical School and Brigham and Women’s Hospital in Boston who was not involved in the studies. And unlike the people who developed the clots before officials pinpointed the link, “we can diagnose it faster and treat it more appropriately if it does happen, so that the outcomes will be better.”
That’s because the vaccine-induced clots are similar to a condition called heparin-induced thrombocytopenia, or HIT. Patients with HIT develop blood clots when treated with the commonly used anti-coagulant drug heparin. Heparin attaches to the PF4 protein, and some people develop an immune response that attacks the two molecules.
Treating vaccinated patients who have PF4 antibodies with heparin is like “adding fuel to the fire” and may cause them to develop more clots, Connors says. Four of the six U.S. women who developed clots after getting the Johnson & Johnson vaccine, for instance, received heparin, as did the man in the clinical trial. The man recovered and one woman was discharged from the hospital. Three were still hospitalized as of April 14. Read more from SN
Subscribe here
What Exactly Are Blood Clots?
The following written content from Richard N. Fogoros, MD
A blood clot, also called a thrombus, is blood that has coagulated or clotted. While clotting is crucial in some circumstances—healing a skin wound by forming a scab, for example—blood clots that occur within arteries or veins can be dangerous and even life-threatening if they block the flow of blood to essential organs, including the heart, lungs, and brain.
:max_bytes(150000):strip_icc():format(webp)/overview-blood-clots-1745326_final-3990f6d12e19428e8734d92f068ce0de.png)
Blood Clot Symptoms
The signs and symptoms of a blood clot depend on whether the clot is in an artery or a vein and wherein the body it is located. A clot in an artery may bring on moderate to severe pain that develops quickly, for example. If a vein is affected, the pain is likely to be milder and to increase in severity over several hours or even days.
Any blood clot may cause swelling, tingling, tenderness, or a feeling of warmth.
If an artery that leads to the brain is clogged, neurological symptoms such as confusion or paralysis can occur, possibly indicating a stroke. A blood clot in the leg might cause the leg to swell so that it’s noticeably larger than the other leg and may be a sign of DVT. If a blood clot forms in the coronary artery, symptoms of a heart attack—including tightness in the chest or arms, dizziness—may occur.1 Signs and Symptoms of a Blood Clot
Causes
All injuries cause damage to blood vessels. When you get a bruise, it’s because a blood vessel was damaged, causing blood to leak out and become visible under the skin. A clot then forms inside the blood vessel; without this process, minor injuries could cause uncontrolled bleeding.
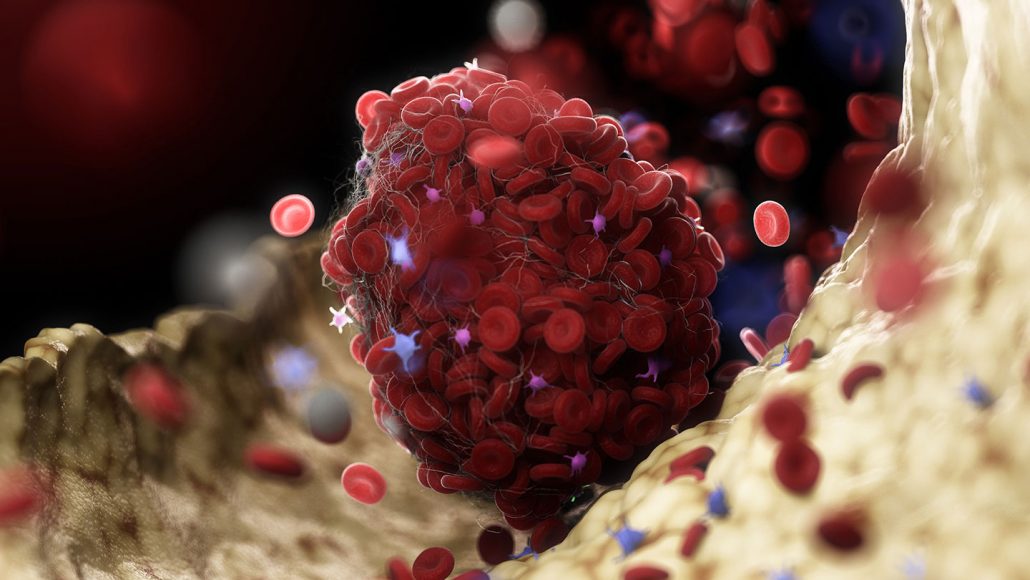
Blood clots are made up of two elements: platelets and fibrin. Platelets are cells produced in the bone marrow that travel throughout the bloodstream. When bleeding occurs, the platelets become sticky, allowing them to adhere to each other and the blood vessel walls.
Fibrin is a substance that resembles a long, sticky string. Strands of fibrin stick to blood vessel walls and clump together to form a web-like complex that red blood cells become caught up in. A blood clot consists of platelets and fibrin strands, as well as trapped red blood cells. The strands of fibrin bind the platelets together and essentially tighten the clot to make it stable.
The clotting mechanism also can cause clots to form in ways that are harmful—a condition called thrombosis.
If a blood clot blocks an artery to the heart, the result can be a heart attack. If blood to the brain is blocked, the result can be a stroke.
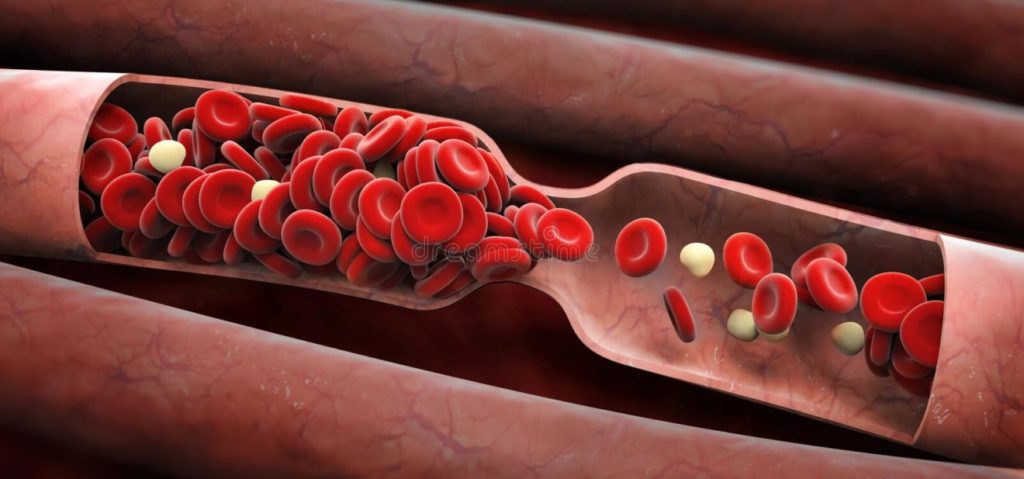
Arteries get smaller and smaller as they move away from the heart, so a clot that starts near the heart will eventually lodge in a smaller vessel. This prevents oxygenated blood from reaching any areas fed by that artery. Embolic strokes, the most common type of stroke, for example, are caused by blood clots traveling to the brain and starving brain tissue of blood and oxygen.
Veins, on the other hand, get larger as they return blood to the heart, so blood clots that form in veins can travel all the way to the heart and then get pumped into the lungs, where they can create a life-threatening condition called a pulmonary embolism. They can also lodge in blood vessels, most commonly in the legs; when this happens, it is called deep vein thrombosis (DVT).
There are numerous risk factors that can predispose you to develop a potentially dangerous blood clot, including:3
- Atrial fibrillation, a condition that causes an irregular heartbeat
- Atherosclerosis, a buildup of plaque in the arteries
- Certain genetic disorders, such as factor V Leiden mutation (FVL)
- Certain medications, such as oral contraceptives and hormone therapy drugs
- Heart arrhythmias (heart rhythm problems)
- Heart failure
- Obesity
- Peripheral artery disease
- Pregnancy
- Prolonged sitting or bed rest
- Smoking
- Surgery
Blood Clot Causes and Risk Factors
Diagnosis
A variety of diagnostic tests are used to detect blood clots, depending on your symptoms and the likely location of the clot. They include:
- D-dimer blood test: This measures a substance in the blood that can detect whether there is abnormal clotting activity somewhere in the bloodstream.
- Cardiac biomarker blood test: This is a blood test that can detect damage to the heart muscle and is used to diagnose a heart attack.
- Compression ultrasound: This is a noninvasive test that can be performed at the bedside and is often very useful in diagnosing DVT.
- V/Q scan: A ventilation-perfusion scan (V/Q scan) uses a radioactive dye to examine blood flow to the lungs and can detect whether a pulmonary blood vessel has been blocked by a pulmonary embolus.
- CT scan: This is often the first test used to diagnose a stroke. It is also useful for confirming a pulmonary embolus.
- MRI scan: MRI scans can be used to detect clots in blood vessels.
- Angiography or venography: These are catheterization techniques in which a dye is injected into a blood vessel where a clot is suspected; X-rays are then taken to detect the clot.
- Echocardiography: Echocardiograms use sound waves to get images of your heart and are often used in patients who have had embolisms affecting an artery—especially in people who have had an embolic stroke. To get into an artery, in almost every case, an embolism will have to either originate within the heart or travel through the heart. Read more from Very Well Health